When I usually
go out of the house you will usually see me all put together nicely. Makeup done, hair done, etc. I have learnt how to hide behind little
tricks to look very presentable with very little effort. These little tricks are to act like a normal
person despite being ill. You will see
me smile even when I am in excruciating agony and possibly dosed up on pain
killers. My body is yelling at me even
though I am hiding what I am feeling and thinking. I do this to act like I am normal. I do it to feel normal too. This is all to hide from others so they do
not know I am suffering in agony and so they do not focus on me being sick as
most people do not know how to respond without hurting me.
Very few people
see me at my lowest (which is my worst days) as I usually hide them very well
now. However, this is not always the
case as some of my very close friends know when I am lying so if they ask me a
question and I usually reply the exact same answer time and time again they now
know that I am hiding something whether it be my Crohn’s hurting me or my
anxiety or depression getting to me. My little
girl Alisha also knows when I am hiding something from her so she has started
bringing me a teddy and giving me a huge slobbery kiss and hug but that is
usually when she sees me slipping with my guard as it does get really tough
keeping my guard up all day. During a
flare up of any of my illnesses whether it be the Crohn’s disease, anxiety or
Fibromyalgia, the last place my body wants me to do is go outside of the house,
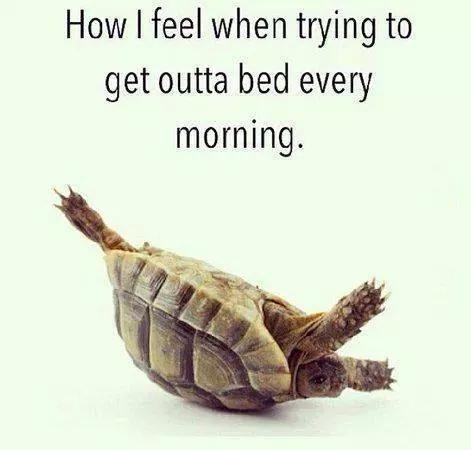
plaster a fake smile on my face an look presentable. On my worst days I actually struggle to get
out of my bed and Alisha actually comes into my bedroom now and says “up mummy
up”. She may only be 2years old but she
knows that the day must go on even if mummy is poorly and wants to stay in bed
all day, so instead we have a pyjama day instead hiding away from everyone.
On my bad days
I only go out of the house if I desperately need to go out so anything like
appointments, work or a food shop is when I only leave the house. On a terrible day I do not even leave my
garden or house depending what the weather is like outside. When I do go outside I need to make sure I
feel safe or there is toilets which are close by just encase I need to run to
them quickly. These places I need to
feel safe because I do not need to explain myself if I have an accident or they
are understanding. I do not do this
because I feel ashamed of my day to day reality, I do this because I sometimes
need protection from the vulnerability I am experiencing. At the end of the day it usually leads to
people’s misconceptions about how bad my illnesses are. There are days I could have a shower and I am
out of breath but I do not let anyone know, but it does not mean I do not
experience this. There can also be days
when my hands shake or I cannot get my feet to move or my face turns a grey
colour as I cannot swallow something or I am trying to catch my breath. You might not see these things happen as you
are busy or just because I hide them from everyone or I do not speak about it
to anyone. YES these days do exist and I
can promise you they do exist. There are
also days I am curled over in agony because I have ate or drank something that does
not agree with my stomach and only a selected amount of people are aware of
this happening. Or I am frozen with
anxiety and I cannot actually move from where I am standing. This happened the other day as I was promised
a lift home after I had finished work to collect Alisha from the
childminders. But that person text
really late and my anxiety had kicked into overdrive and that made me freeze to
a spot near work because I knew I would have been collected safely after
arriving to work and the whole shopping centre was evacuated due to a bomb
alert. I did have the choice of going
home and saying I am not working but after the police had gave everyone the all
clear to return to work I said to myself that anxiety you are not getting the
better of me as I am in control not you.
Bad days and terrible days do happen to people with chronic illnesses but those who suffer with more than one chronic illness can suffer with more bad or terrible days depending on if the illnesses are in remission and under control. However, there can be a day when that illness decides to say oh no you are going to be tortured today and I am going to make your day hell.